Quality Improvement Plan
Quality Improvement Plan 2025/2026
Perley Health is a not-for profit seniors' care organization with 450 provincially licensed long-term care beds. While Perley Health's primary focus is on long-term care, it also actively supports the capacity of seniors to live independently. To this end, Perley Health partners effectively with like-minded organizations across the continuum of care to develop a community of care and to provide ready access to a range of clinical and therapeutic services, along with social and recreational activities.
Perley Health is pleased to share its 2025/26 Quality Improvement Plan (QIP). Our ongoing commitment to quality is reflected in our mission “to achieve excellence in the health, safety and well-being of Seniors and Veterans with a focus on innovation in person-centred and frailty-informed care and service" and in our long-term strategic plan, which identifies Excellence in Resident Care and Service as one of Perley Health's four key strategic pillars. In 2021, Perley Health's strategic plan was refreshed in response to several unprecedented factors which resulted in a fundamentally changed healthcare landscape. These factors included, amongst others, the ongoing impacts of the COVID-19 pandemic, persistent healthcare worker shortage and burnout, increased public attention on long term care, and increased regulation of an already highly regulated environment. The core pillars of the long-term strategy remain relevant, and are reflected in the interim strategy which outlines objectives and priorities for 2022 - 2025. These objectives include "Sustaining excellence in Seniors' and Veterans' care", as well as embodying a "People First" philosophy. The QIP is a roadmap to achieving both objectives, while navigating challenges and opportunities in our environment..
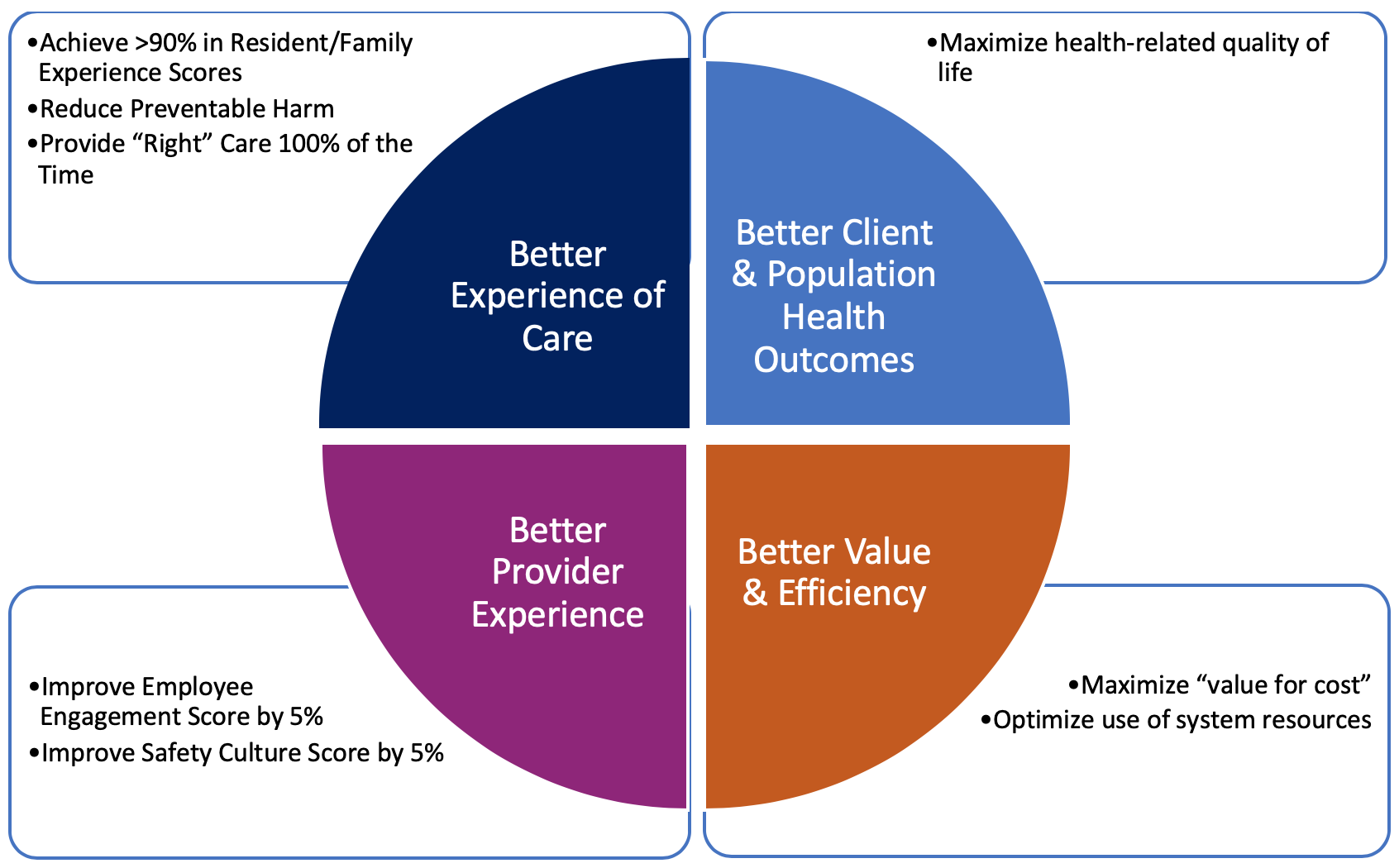
Perley Health's QIP is aligned with our Quality Framework, based on the Quadruple Aim framework adopted by Ontario Health. The high-level priorities for this year's QIP are informed by the quality and safety aims under the various pillars of the framework, as determined by Perley Health's Board of Directors:
- increase resident and family experience
- reduce preventable harm
- provide the “right care” 100% of the time improve health-related quality of life
- improve the provider experience
Annual quality priorities, targets for improvement and projected change ideas/tactics reflect:
- progress achieved in recent years;
- the most recent performance data available from the Canadian Institute for Health Information (CIHI), resident, family and staff experience surveys and our electronic health record;
- emergent issues identified internally (trends in critical incidents) and/or externally;
- input from residents, families, staff, leaders and external partners, including the MOLTC.
Quality Objectives for 2025-2026 are divided into two categories – focused action and moderate action.
Focused action
- Improve the staff experience by continuing to implement People First initiatives. Work in this area will focus on enhancing Employee Engagement, Diversity, Equity and Inclusion, Workplace safety and Wellbeing.
- Improve the experience of residents by continuing to focus on enhancing opportunities for activation and engagement as well as mealtimes. New work in this area will include a focus on enhancing resident perceptions of staff responsiveness.
- Improve the experience of residents and family members by focusing on person-centred communication. Anticipated work for this cycle includes development and implementation of a post-admission communication plan as well as a re-design of care conferences in collaboration with residents/families.
Moderate action
- Enhance pain assessment and management practices. Work will focus on sustainability and spread of the PainChek mobile application to increase quality of pain assessment for residents with cognitive and communication challenges; as well as strengthening our approach to non-pharmacological pain management.
- Optimize antipsychotic use. Focus on sustaining interprofessional approach to regularly review and evaluate antipsychotic use aligned with best practice to ensure maximum therapeutic benefit and minimize negative outcomes.
- Enhance person-centred care at end-of-life. Continue to build capacity across interprofessional team through enhanced palliative and end-of-life care training opportunities. Strengthen new and existing supportive processes to ensure consistent, quality care at end-of-life.
- Minimize potentially avoidable emergency department transfers. Work in this area will be aligned with other priority areas, including person-centred care and communication, and end-of-life care. Work will focus on enhancing key practices to better support provision of care aligned with resident/family goals of care following an acute health event, or at end-of-life.
-
Download the 2025 – 2026 Quality Improvement Plan
-
Download the 2025 – 2026 Quality Improvement Plan Narrative
-
Download the 2024 – 2025 Continuous Quality Improvement Annual Report
Archive:
Contact Information
Melissa Norman,
Director, Quality and Interprofessional Care
Email: mnorman@perleyhealth.ca
Phone: 613-526-7170 ext. 2448